[ad_1]
Scientists at the Research Institute of the McGill University Health Centre (RI-MUHC) have identified new means of fighting drug-tolerant bacteria, a growing global threat as menacing as drug-resistant microbes. Little is known about the mechanisms leading to tolerance, a strategy that makes bacteria “indifferent” to antibiotics and almost “un-killable,” which results in chronic infections extremely difficult to treat and cure.
The RI-MUHC’s research team discovered a new cellular target that can weaken the bacterium Pseudomonas aeruginosa, a daunting microbe which can become highly tolerant to many antibiotics, and thus refractory to antibiotic therapy. The team’s findings are published this week in the Proceedings of the National Academy of Sciences (PNAS).
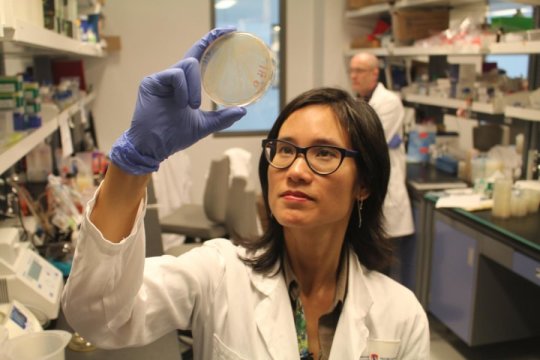
“We identified a new function important to antibiotic tolerance, which could be targeted to enhance the activity of our current antibiotics,” says lead study author Dr. Dao Nguyen, a scientist from the Translational Research in Respiratory Diseases Program at the RI-MUHC and an associate professor of Medicine at McGill University. “This is critical if we want to improve the efficacy of our antibiotics and prevent such treatments from failing.”
P. aeruginosa lung infection ,is the leading cause of death for thousands of people living with cystic fibrosis. This bacterium also causes many other serious infections in which in people with weakened defenses and immune system.
“P. aeruginosa causes lifelong lung infections in individuals with cystic fibrosis, and these infections cannot be cleared, even by cocktails of the most potent antibiotics available,” says Dr. Nguyen, who is also a respirologist at the McGill University Health Centre.
A “Nightmare bacteria” that grows slowly
P. aeruginosa has been listed among the “nightmare bacteria” by the Centers for Disease Control and Prevention (CDC) in the United States, with an estimated 51,000 healthcare-associated infections each year resulting in around 400 deaths. It is a common cause of healthcare-associated infections such as pneumonia, bloodstream or urinary tract infections, and surgical site infections
“Many bacteria, such as P. aeruginosa, when they grow slowly or do not grow at all, become tolerant to antibiotics,” explains Dr. Nguyen. “This is a crucial problem because many chronic infections are caused by bacteria that are slow growing or enter a dormant state when they reside in a living host, and this causes treatments to fail or infections to relapse in patients.”
A new enzyme target for antibiotics
In this newest research, Dr. Nguyen and her team have discovered that when P. aeruginosa is under stress or lacking nutrients, it uses a stress signaling system and defense enzyme (superoxide dismutase) to modify its cell membrane, making it less permeable to molecules and preventing antibiotics from penetrating the cell.
Researchers found that inhibition of the enzyme activity or the stress signaling system could render the pathogen more susceptible to antibiotics.
“Up until now antibiotic tolerance in slow growing bacteria was widely attributed to the fact that targets of antibiotics were not available or inactive in ‘dormant’ cells. With this research we have shown there is more to it than that” explains Dr. Nguyen. “We identified a new link between the stress defense enzyme, the regulation of membrane permeability and antibiotic tolerance.”
“In the long run, the discovery of this promising cellular target could expand the utility of our antibiotics and make new ones more effective,” she concludes.
Story Source:
Materials provided by McGill University Health Centre. Note: Content may be edited for style and length.
[ad_2]