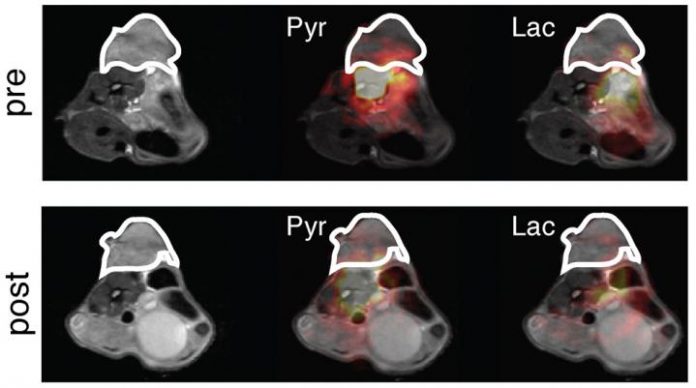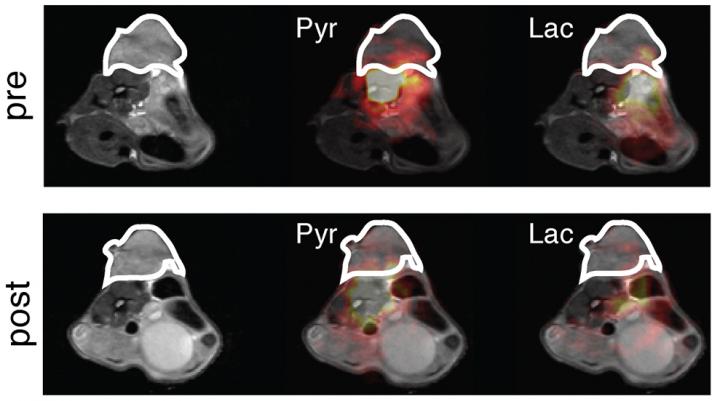
Photo: False colour image of a breast tumour (outlined) pre- and post-treatment with a PI3Ka inhibitor. Weaker colours post-treatment indicate that the drug is working.
view more
Credit Image: Brindle Lab, University of Cambridge
Imaging techniques could replace the need for invasive tissue biopsies in helping rapidly determine whether cancer treatments are working effectively, according to researchers at the University of Cambridge.
In a study published in the journal Cancer Cell, researchers at the Cancer Research UK (CRUK) Cambridge Institute have shown how a new technique known as hyperpolarisation – which involves effectively magnetising molecules in a strong magnetic field – can be used to monitor how effective cancer drugs are at slowing a tumour’s growth.
In healthy tissue, cell proliferation is a tightly controlled process. When this process goes wrong, cell proliferation can run away with itself, leading to unchecked growth and the development of tumours.
All tissue needs to be ‘fed’. As part of this process – known as metabolism – our cells break down glucose and other sugars to produce pyruvate, which is in turn converted into lactate. This is important for producing energy and the building blocks for making new cells.
Tumours have a different metabolism to healthy cells, and often produce more lactate. This metabolic pathway is affected by the presence of a protein known as FOXM1, which controls the production of a metabolic enzyme that converts pyruvate into lactate. FOXM1 also controls the production of many other proteins involved in cell growth and proliferation.
Around 70% of all cases of breast cancer are of a type known as estrogen-receptor (ER) positive. In many ER-positive breast cancer cases, an enzyme known as PI3K? is activated. This leads to an abundance of FOXM1, enabling the cancer cells to grow uncontrollably – the characteristic sign of a tumour cell.
Drugs that inhibit PI3K? are currently being tested in breast cancer patients. Such drugs should be able to decrease the amount of FOXM1 and check the tumour’s growth. However, a patient’s tumour may have an innate resistance to PI3K? inhibitors, or can acquire resistance over time, making the drugs increasingly less effective.
Dr Susana Ros, first author from the CRUK Cambridge Institute, said: “Thanks to advances in cancer treatments, our medicines are becoming more and more targeted, but not all drugs will work in every case – some tumours are resistant to particular drugs. What we need are biomarkers – biological signatures – that tell us whether a drug is working or not.”
The researchers took breast cancer cells from patients and grew them in mouse ‘avatars’ to allow them to study the tumours in detail. They found that in tumours resistant to PI3K? inhibitors, cancer cells continue to produce FOXM1 – meaning that this molecule could be used as a biomarker for drug resistance in patients with ER-positive breast cancer.
Checking whether a tumour is continuing to produce FOXM1 – and hence whether the PI3K? inhibitor is still working – would usually involve an invasive tissue biopsy. However, researchers have used a new imaging technique to monitor this in real time and non-invasively.
The technique developed and used by the team is known as hyperpolarisation. First, the team produces a form of pyruvate whose carbon atoms are slightly heavier than normal carbon atoms (they carry an additional neutron and are hence known as carbon-13 molecules). The researchers then ‘hyperpolarise’ – or magnetise – the carbon-13 pyruvate by cooling it to around one degree above absolute zero (-272°C) and exposing it to extremely strong magnetic fields and microwave radiation. The frozen material is then thawed and dissolved into an injectable solution.
Patients are injected with the solution and then receive a regular MRI scan. The signal strength from the hyperpolarised carbon-13 pyruvate molecules is 10,000 times stronger than that from normal pyruvate, making the molecules visible on the scan. The researchers can use the scan to see how fast pyruvate is being converted into lactate – only the continued presence of FOXM1 would allow this to happen, and this would be a sign that the drugs are not working properly.
Dr Ros added: “We’ve been able to detect the presence of FOXM1, our biomarker, by using this new imaging technique in breast cancer models to look for a proxy – that is, how quickly pyruvate is converted to lactate.”
Professor Kevin Brindle, senior author of the study, commented: “In the future, this could provide us with a rapid assessment of how a breast cancer patient is responding to treatment without the need for invasive biopsies. This information could help put an end to giving treatments that are not working and the side effects that accompany them. Currently, patients can wait a long time to find out if a treatment is working. This technique could shorten this time, and help to tailor treatment for individual patients.”
###
Reference
Ros, S et al. Metabolic Imaging Detects Resistance to PI3Kα Inhibition Mediated by Persistent FOXM1 Expression in ER+ Breast Cancer. Cancer Cell; 24 Sept 2020; DOI: 10.1016/j.ccell.2020.08.016
TDnews (tunisiesoir.com)