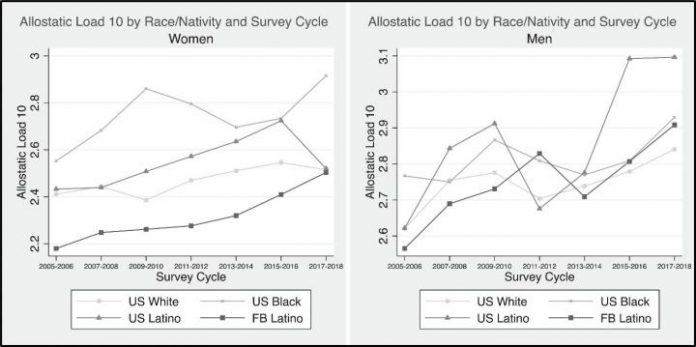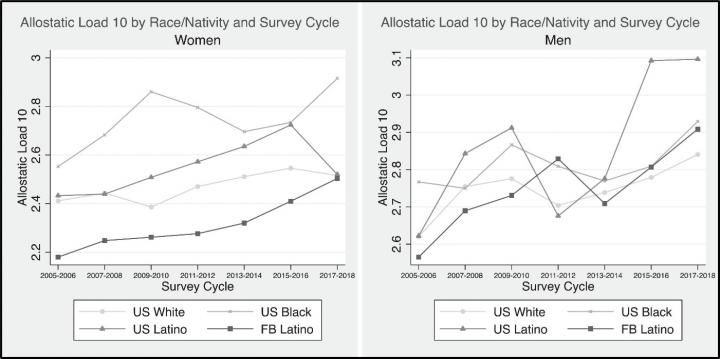
Photo: These figures show predicted values of allostatic load for women and men for each race/nativity group by survey cycle between 2005 to 2018.
view more
Credit Image: American Journal of Preventive Medicine
Ann Arbor, December 15, 2020 – Structural racism can lead to discrimination in many aspects of life including criminal justice, employment, housing, health care, political power, and education. A new study published in the American Journal of Preventive Medicine examines the impact of structural racism on health and confirms that chronic exposure to stressors leads to a marked erosion of health that is particularly severe among foreign-born Blacks and Latinx. Investigators say largescale structural policies that address structural racism are needed.
Structural racism is defined as laws, rules, or official policies in a society that result in a continued unfair advantage to some people and unfair or harmful treatment of others based on race. “There is evidence that structural racism has a material impact on the health of racial/ethnic minorities and immigrants,” explained lead investigator Brent A. Langellier, PhD, Department of Health Management and Policy, Dornsife School of Public Health, Drexel University, Philadelphia, PA, USA. “Comparing allostatic load–a multidimensional measure of the body’s response to stressors experienced throughout the life course–between immigrants and non-immigrants of different racial/ethnic backgrounds can help shed light on the magnitude of health differences between groups.”
Investigators examined patterns in allostatic load among US- and foreign-born Whites, Blacks, and Latinx. Using data from the 2005-2018 National Health and Nutrition Examination Survey (NHANES), they collected data on a 10-item measure of cardiovascular, metabolic, and immunologic risk. Measures of cardiovascular risk included systolic blood pressure, diastolic blood pressure, total cholesterol, and high-density lipoprotein cholesterol. Metabolic risk indicators included body mass index (BMI), blood sugar (HbA1c), urinary albumin, and creatinine clearance. Immunologic measures were white blood cell count and current or previous asthma diagnosis. Based on the literature suggesting that, for many outcomes, immigrants have paradoxically good health that declines with time in the US, investigators examined aging gradients in allostatic load for each group. They also assessed whether allostatic load in each group changed across NHANES survey cycles. Their analyses were conducted in March 2020.
Results showed that allostatic load increased with age among all groups, but the increases were much steeper among foreign-born Blacks of both genders and foreign-born Latina women. The difference between the first and last survey cycle was most pronounced among US-born Black women (from 2.74 in 2005-2006 to 3.02 in 2017-2018), US-born Latino men (from 2.69 to 3.09), and foreign-born Latino men (from 2.58 to 2.87). Aging gradients in allostatic load were steepest among foreign-born Blacks of both genders and foreign-born Latina women, and flattest among US-born and foreign-born Whites. Notably, foreign-born Latina women had among the lowest allostatic load at the youngest ages but among the highest at the upper end of the age distribution.
“Our findings add to the evidence that structural racism has a material impact on the health of racial/ethnic minorities and immigrants – and that this effect accumulates throughout the life course,” noted Dr. Langellier. “They further suggest that the disadvantage experienced by racial/ethnic minorities is compounded among minorities who are also immigrants, which erodes the health advantage that many immigrants have at early ages.”
These findings highlight the magnitude of the disparities in health that are produced by inequities in exposure to these risk and protective factors. “Collectively, our findings and evidence in the broader literature suggest that reducing these disparities will require big, structural policies that address structural racism, including inequities in upstream social determinants of health,” concluded Dr. Langellier.
###
TDnews (tunisiesoir.com)