New research by UCLA Jonsson Comprehensive Cancer Center investigators has found further proof that melanoma cells, which are a deadly type of skin cancer, can spread throughout the body by creeping like tiny spiders along the outside of blood vessels without ever entering the blood stream. In addition, they found that this process is intensified by exposure to ultraviolet light. Therefore, they are searching for a new drug can counteract this process.
The new study was based on the pioneering work of Dr. Claire Lugassy and Dr. Raymond Barnhill at UCLA’s Jonsson Comprehensive Cancer Center. Their team of resesearchers collaborated with a team from the University of Bonn, Germany, led by Dr. Thomas Tuting. The study authors note that it is well-known that melanoma cells can spread through the blood to accumulate and form new tumors (metastases) in other parts of the body; thus, a small skin cancer can metastasize to the brain, lungs, liver, or other organs. Almost two decades ago, Drs.
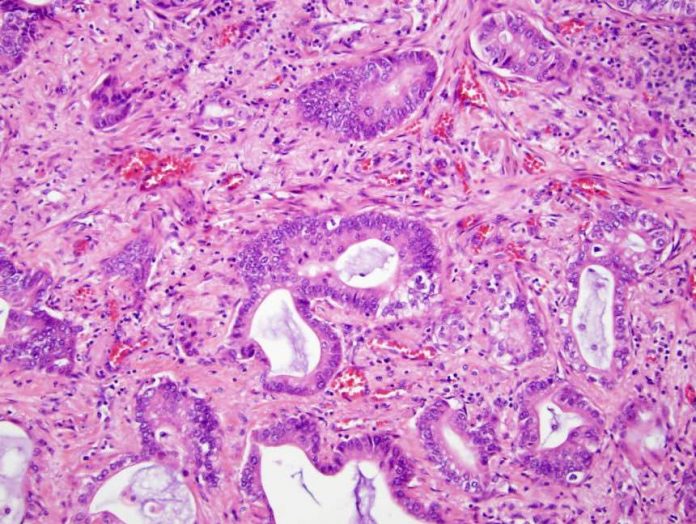
Lugassy and Barnhill began studying the way cancer, especially melanoma, metastasizes; they conceived and developed a process, which they dubbed extravascular migratory metastasis (EVMM). They found that, in addition to traveling in the bloodstream, melanoma cells could also move along the abluminal, or outside, surface of blood vessels; they accomplish this by a process known as angiotropism, which is a biological interaction between the cancer cells and the blood vessel cells. Drs. Lugassy and Barnhill are continuing to accumulate evidence that confirms the reality of this metastatic pathway of cancer cells.
Via angiotropism and EVMM, the melanoma cells may replace a type of cell called a pericyte, which is normally present on the outsides of blood vessels. While imitating the tendril-like pericytes (Drs. Lugassy and Barnhill term this pericytic mimicry), the melanoma cells creep along the length of blood vessels like spiders until they reach a distant area where they accumulate to form new tumors.
Dr. Lugassy noted, “At first our idea was controversial, but mounting evidence confirming angiotropism and EVMM has revolutionized the knowledge of how cancer spreads through the body to the point that other scientists have confirmed the process in other solid tumor cell types such as pancreatic cancer.” In the new study, the researches again observed EVMM in a genetically engineered mouse model. The investigators also discovered that when the mice with melanoma were exposed to ultraviolet radiation their immune systems responded with inflammation that accelerated the angiotropism; thus, increasing the amount of EVMM, and leading to more lung metastases in the mice than those not exposed to ultraviolet light. This component of the study was conducted in the Laboratory for Experimental Dermatology in Bonn, Germany, under the direction of Dr. Tuting. Dr. Barnhill explained, “We have known for a long time that UV radiation is a factor in the development of melanoma, but in this study the melanoma was already present in the mice.” Dr. Tuting observed that UV light provoked inflammation at the site of the tumor, which caused the mouse immune system to attract neutrophils (a type of white blood cell), and the neutrophils promoted angiotropism. The investigators note that with their new knowledge, they can now begin searching for a drug target that will interfere with this EVMM process; their goal is to create a treatment that would stop EVMM. Because the danger of melanoma comes from its metastasis from the skin to vital organs, being able to slow down or stop metastasis could turn a disease that is often fatal into a manageable chronic illness with relatively little risk of death.