Huntington’s disease is a progressive and fatal neurologic disorder that is caused by a mutant gene. It strikes in adulthood and affects 1 in every 10,000 Americans, while another 250,000 are at risk because they carry the inherited gene mutation. UCLA researchers have discovered that the removal of a specific molecular switch from a mutant protein can trigger symptoms in mice, which are similar to those found in human with Huntington’s disease. The study, which was published on the current online edition of the journal Neuron, provides further insight into how Huntington’s disease evolves.
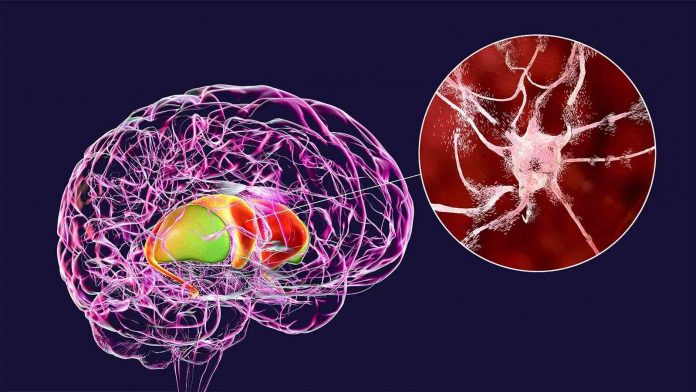
Symptoms of Huntington’s disease include chorea (jerky, uncontrollable movements), dystonia (continued involuntary muscle contractions) and an abnormal gait that can result in frequent falls. People with the disease also suffer from debilitating cognitive and psychiatric deficits; they typically die of complications from Huntington’s disease about 20 years after symptoms first appear. Most of the individuals with the genetic defect do not have any symptoms until middle age; as a result, they often unknowingly pass on the mutated gene to their children. These symptoms, which also appear in the adult mice used in the study, included chorea-like and dystonia-like movement deficits, progressively worsening gait with spontaneous falls, and atrophy and neuronal cell loss in specific brain regions.
The study was led by X. William Yang, MD, PhD, a UCLA professor of psychiatry. his team genetically engineered a small area on the huntingtin protein known as N17. They found that this resulted in a significant suppression of the disease in an earlier mouse model of Huntington’s disease that they had developed. The research led to the question that formed the basis of the new study: If the N17 domain could alter the mutant gene in a positive manner, what would happen if the N17 area function were completely abolished? To attain the answer, the researchers developed a new mouse model with the N17 area completely removed; this allowed them to unravel the molecular function of that part of the protein that causes the disease in mice.
“Although we did expect the mouse model to exhibit somewhat more severe disease symptoms compared to our previous Huntington’s disease mice, we were surprised to discover that deleting the domain in the new mice caused multiple disease-like symptoms and neuronal cell loss that are reminiscent of those found in Huntington’s patients,” explained first author Xiaofeng Gu, MD, PhD, an assistant researcher in Dr. Yang’s lab. Dr. Yang noted that their new mouse model provides important clues regarding how a normally functioning N17 area might protect neurons in the brain against the disease, Compared to similar mice with an intact N17 area, the mice lacking N17 showed a significantly more rapid accumulation of mutant huntingtin, which appears as clumps in the nuclei of brain cells.
Dr. Yang explained, “This study makes clear that a major neuroprotective function of N17 is to prevent the mutant protein from entering the nucleus and eliciting more severe toxicities.” He added that the result is consistent with findings from several studies of other, similar neurologic disorders in which mutant proteins with expanded glutamine in the nucleus are key for initiating the disease process. The investigators also found that the mice experienced inflammation in the brain somewhat similar to that found in people with Huntington’s. “Neuroinflammation is emerging as a potentially shared mechanism in multiple neurodegenerative disorders, including Alzheimer’s disease, Parkinson’s disease and amyotrophic lateral sclerosis, and the mouse model shows similar inflammation to that found in both Huntington’s and Alzheimer’s,” explained Dr. Yang. He added, “So these mice may have the potential to be used to study disease mechanisms and test neuroprotective or anti-inflammatory therapeutics for these various disorders.”
The research team next plans to focus on unraveling the detailed molecular pathways that function through N17 to regulate trafficking the huntingtin protein between the cytoplasm (cell tissue) and their nuclei, and test whether targeting these pathways could prevent the onset or slow the progression of the disease in mouse models of Huntington’s.