When I began my practice in obstetrics and gynecology, the majority of my colleagues used sutures and some used skin clips. Later, staples (similar to the ones used to fasten paper together) came into use. I was never an advocate of clips or staples and preferred placing a subcuticular (below the skin) dissolvable suture. My reasoning was that it avoided the discomfort of staple removal and produced a good cosmetic result. A new study compared staples to suture for skin closure after a cesarean section—and suturing was found to be superior. The findings were published in the June issue of the journal Obstetrics & Gynecology.
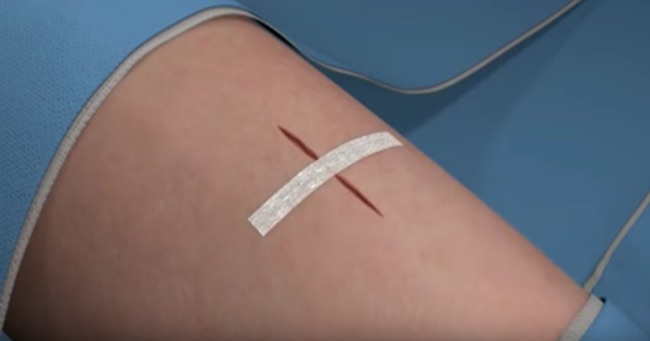
The study authors note that in the US, 33% of all deliveries were performed by cesarean (1.3 million cesarean deliveries per year). The cesarean delivery rate in China has been reported to be as high as 46%. Despite being the most common major operation performed annually in the US, the authors note that data is extremely limited regarding the best practices for closure of the cesarean delivery skin incision. In most cases, a cesarean delivery is performed through a suprapubic low-transverse skin incision (bikini cut). At the conclusion of the surgery, the skin incision is typically closed with the placement of either a continuous subcutaneous suture that dissolves over time or multiple metal staples that are removed at a later date.
The authors cite a recent Cochrane review that compared suture with staples for cesarean delivery skin closure; that study concluded that future studies were needed that take into consideration the effect of body mass index (BMI) and primary compared with repeat cesarean delivery. That study noted that future studies to evaluate the optimal surgical techniques to decrease the risk of wound complications. Therefore, the objective of the present study was to evaluate whether the wound complication rates after cesarean delivery differed between women whose skin incisions were closed with suture, compared with staples.
The investigators conducted a prospective (forward-looking), randomized clinical trial conducted at three US hospitals. It comprised women undergoing cesarean delivery at 23 weeks of gestation or greater via a low-transverse skin incision. The women were randomized to closure of the skin incision with suture or staples; they were also segregated by BMI and primary vs. repeat cesarean delivery. The primary outcome measurement was the incidence of wound complications: infection, hematoma (pocket of bloody fluid), seroma (pocket of non-bloody fluid), separation of 1 cm or longer, or readmission for wound complications.
The study group comprised 746 women (suture: 370; staple: 376). The average gestational age was 39 weeks. A total of 58 women (7.8%) suffered wound complications; 4.9% in the suture group and 10.6% in the staple group. The researchers noted that these wound complications were primarily the result of the decreased incidence of wound separation in the suture group (1.6% vs. 7.4%).
The authors concluded that suture closure of the skin incision at cesarean delivery is related to a 57% decrease in wound complications compared with staple closure.