[ad_1]
Scientists have discovered that some treatments for cancer and sickle cell disease can destroy the germ cells that go on to develop into sperm in the testes of young boys. In some pre-pubescent boys, the treatment for sickle cell disease results in complete destruction of all their germ cells, which are called spermatogonia.
The study, which is published in Human Reproduction, is the first to describe the effects of these treatments on spermatogonial quantity, although boys who have undergone chemotherapy or radiotherapy are known to be at risk of reduced fertility in adulthood.
As a result of their findings, the researchers say that if doctors plan to remove and freeze testicular tissue for fertility preservation, this should be performed before boys undergo a type of chemotherapy that uses high doses of drugs called ‘alkylating agents’. This would give the boys some hope of restoring their fertility when they become adults. Before puberty, boys are usually unable to produce sperm samples that can be frozen and preserved for a time when they might want to start a family. Transplantation of testicular tissue back into the patients after treatment is a possible way of restoring fertility, but, at present, ways to generate sperm from preserved immature testicular tissue are experimental and there have been no pregnancies so far. It may also depend on having sufficient quantities of successfully preserved healthy spermatogonia.
Led by Dr Jan-Bernd Stukenborg, associate professor at the Karolinska Institutet and University Hospital (Stockholm, Sweden), a group of international researchers analysed testicular tissue taken for fertility preservation between 2014 and 2017 from 32 boys with an average age of six, living in Sweden, Finland and Iceland, who were facing treatments that carried a high risk of infertility: testicular irradiation, chemotherapy or radiotherapy as a preparation for a bone marrow transplant because they had cancer or blood disorders such as sickle cell disease, thalassaemia major or Fanconi anemia. Sickle cell disease is the major reason for bone marrow transplantation in children who do not have cancer. Twenty boys had the tissue taken after initial chemotherapy and 12 had it taken before starting any treatment. In addition, they looked at 14 healthy testicular tissue samples stored in the biobank at the Karolinska hospital.
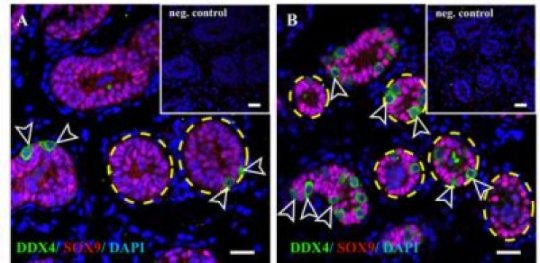
They counted the number of germ cells found in a cross-section of little tubes in the testes where spermatogonia are created, called seminiferous tubules. “We could compare the number of spermatogonia with those found in the healthy boys as a way to estimate the effect of medical treatment or the disease itself on the future fertility of a patient,” explained Dr Stukenborg.
“We found that the numbers of germ cells present in the cross-sections of the seminiferous tubules were significantly depleted and close to zero in patients treated with alkylating agents. The germ cell pool in five boys with sickle cell disease were totally depleted and very low in another; all six had received hydroxyurea. This was not seen in patients who had not started treatment, or were treated with non-alkylating agents, or in the biobank tissues.”
Alkylating agents are used in some chemotherapies, killing cancer cells by damaging their DNA. Hydroxyurea is a chemotherapy agent that is often used to treat the effects of blood disorders such as sickle cell disease, where it improves the function of red blood cells. It reduces the symptoms of the sickle cell disease but is not a cure. Bone marrow transplants offer the best chance of a cure or long-term remission. However, before a transplant, the patient’s own bone marrow has to be destroyed and the immune system suppressed by radiation or chemotherapy so that the body does not reject the transplant from another person.
Co-author, Dr Cecilia Petersen, a senior consultant in paediatric oncology at the Karolinska Institutet, said: “Our findings of a dramatic decrease in germ cell numbers in boys treated with alkylating agents and in sickle cell disease patients treated with hydroxyurea, suggest that storing frozen testicular tissue from these boys should be performed before these treatments are initiated. This needs to be communicated to physicians, as well as patients and their parents or carers.
“However, until sperm that are able to fertilise eggs are produced from stored testicular tissue, we cannot confirm that germ cell quantity might determine the success of transplantation of the tissue in adulthood. Further research on this is needed to establish a realistic fertility preservation technique.”
The authors point out that for some boys the disease itself may have already affected the number of spermatogonia before any treatment has even begun, and so for them preserving testicular tissue may not be a viable option. Co-author, Professor Kirsi Jahnukainen, a senior consultant in paediatric oncology at the Children’s Hospital, University of Helsinki, Helsinki University Central Hospital (Helsinki, Finland), said: “Among patients who had not been treated previously with chemotherapy, there were several boys with a low number of germ cells for their age. This suggests that some non-malignant diseases that require bone marrow transplants may affect the fertility of young boys even before exposure to therapy that is toxic for the testes.”
The researchers say that it is possible for germ cells to recover to normal levels after treatment that is highly toxic to the testes, but that high doses of alkylating agents and radiotherapy to the testicles, including total body irradiation, is strongly associated with permanent or long-term infertility.
Prof Jahnukainen added: “The first group of boys who received bone marrow transplants are now reaching their thirties. Recent data suggest they may have a high chance of their sperm production recovering, even if they received high dose alkylating therapies, so long as they had no testicular irradiation.”
A limitation of the study was that the samples of normal tissue from the biobank had no detailed information regarding previous medical treatments and testicular volumes for these patients.
[ad_2]