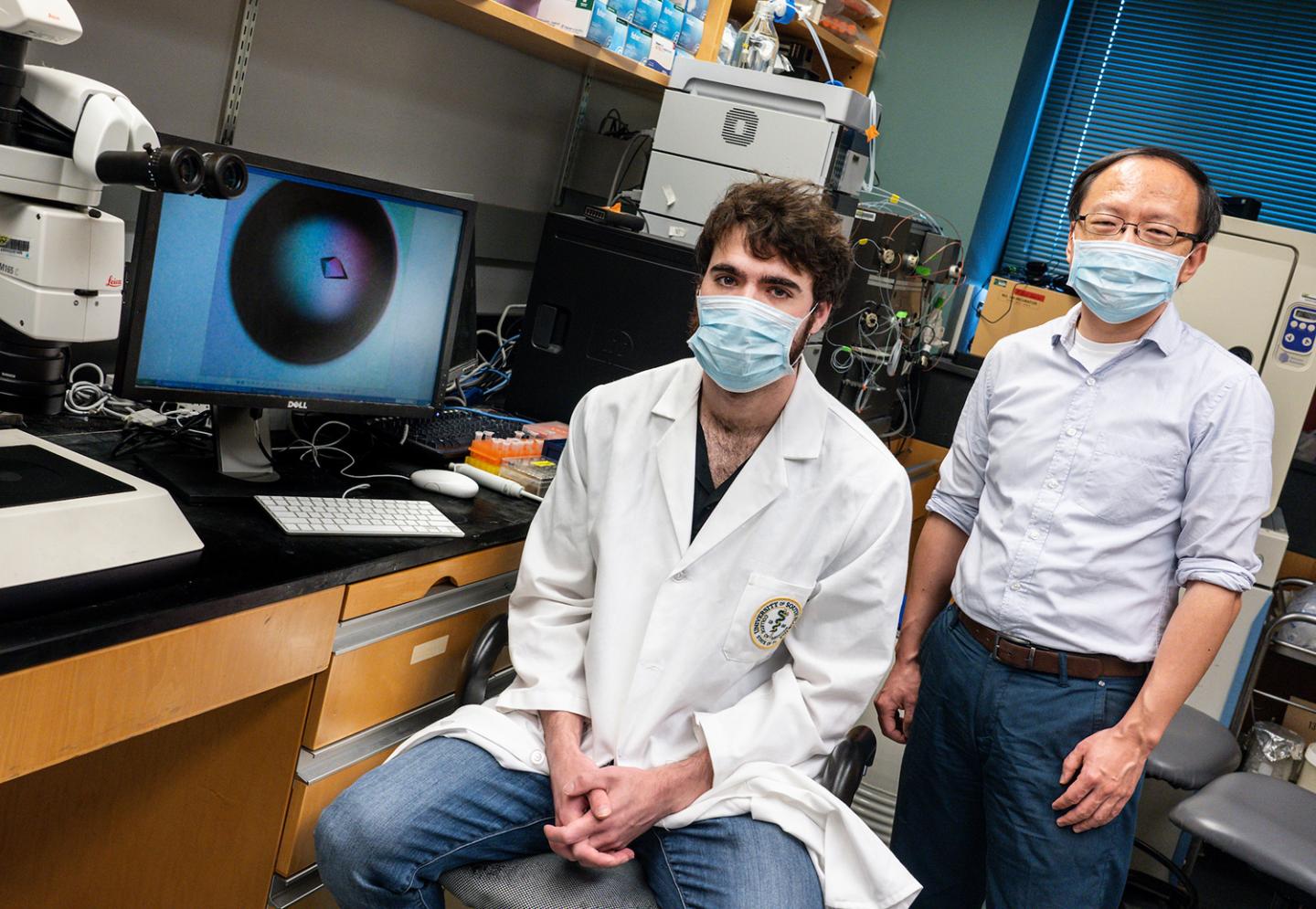
Photo: Lead author Michael Sacco (sitting), a doctoral student in the USF Health Department of Molecular Medicine, with study co-principal investigator Yu Chen, PhD, in Dr. Chen’s laboratory at the University…
view more
Credit Image: Photo courtesy of USF Health/University of South Florida
TAMPA, Fla (Nov. 6, 2020) — SARS-CoV-2, the respiratory virus that causes COVID-19, attacks the body in multiple steps. Gaining entry into cells deep within the lungs and hijacking the human host cell’s machinery to churn out copies of itself are two of the earliest steps — both essential for viral infection.
A new study offers insight into designing antiviral drugs against COVID-19 by showing that some existing compounds can inhibit both the main protease (Mpro), a key viral protein required for SARS-CoV-2 replication inside human cells, and the lysosomal protease cathepsin L, a human protein important for viral entry into host cells. The study, led by researchers at the University of South Florida Health (USF Health) Morsani College of Medicine and the University of Arizona College of Pharmacy, was published today in Science Advances.
“If we can develop compounds to shut down or significantly reduce both processes – viral entry and viral replication – such dual inhibition may enhance the potency of these compounds in treating the coronavirus infection,” said study co-principal investigator Yu Chen, PhD, a USF Health associate professor of molecular medicine with expertise in structure-based drug design. “Metaphorically, it’s like killing two birds with one stone.”
The USF Health-University of Arizona (UA) collaborators built upon their previous work, which identified and analyzed several promising, existing antiviral drugs as candidates to treat COVID-19. All the candidates chosen to pursue target Mpro to block the replication of SARS-CoV-2 within human cells grown in the laboratory.
Two of the compounds, calpain inhibitors II and XII, did not show as much activity against Mpro as another drug candidate called GC-376 in biochemical tests. However, the calpain inhibitors, especially XII, actually worked better than GC-376 at killing SARS-CoV-2 in cell cultures, said lead author Michael Sacco, a doctoral student in Dr. Chen’s laboratory.
“We figured if these calpain inhibitors were less effective at inhibiting the virus’s main protease, they must be doing something else to explain their antiviral activity,” Sacco said. They learned from research done by other groups, including collaborator and study co-principal investigator Jun Wang, PhD, of UA, that calpain inhibitors can block other proteases, including cathepsin L, a critical human host protease involved in mediating SARS-CoV-2 entry into cells.
In this latest study, the USF Health researchers used advanced techniques, particularly X-ray crystallography, to visualize how calpain inhibitors II and XII interacted with viral protein Mpro. They observed that the calpain II inhibitor fit as expected into the targeted binding sites on the surface of the SARS-CoV-2 main protease. Unexpectedly, they also discovered that the calpain XII inhibitor adopted a unique configuration – referred to as “an inverted binding pose” — to tightly fit into Mpro active binding sites. (A snug fit optimizes the inhibitor’s interaction with the targeted viral protein, decreasing the enzyme activity that helps SARS-CoV-2 proliferate.)
“Our findings provide useful structural information on how we can design better inhibitors to target this key viral protein in the future,” Dr. Chen said.
Besides the increased potency (desired drug effect at a lower dose) of targeting both viral protease Mpro and human protease cathepsin L, another benefit of dual inhibitors is their potential to suppress drug resistance, Dr. Chen said.
SARS-CoV-2 can mutate, or change its targeted genetic sequence. These viral mutations trick the human cell into allowing the virus to attach to the cell’s surface membrane and insert its genetic material, and can alter the shape of viral proteins and how they interact with other molecules (including inhibitors) inside the cell.
When the virus mutates so it can continue reproducing, it can become resistant to a particular inhibitor, reducing that compound’s effectiveness. In other words, if the genetic sequence of the viral target (lock) changes, the key (inhibitor) no longer fits that specific lock. But let’s say the same key can open two locks to help prevent COVID-19 infection; in this case the two locks are Mpro, the viral target protein, and cathepsin L, the human target protein.
“It’s harder for the virus to change both locks (two drug targets) at the same time,” Dr. Chen said. “So a dual inhibitor makes it more difficult for antiviral drug resistance to develop, because even if the viral protein changes, this type of compound remains effective against the human host protein that has not changed.”
The USF Health-University of Arizona research team continues to fine-tune existing antiviral drug candidates to iMprove their stability and performance, and hopes to apply what they’ve learned to help design new COVID-19 drugs. Their next steps will include solving how calpain inhibitors interact chemically and structurally with cathepsin L.
###
Jun Wang, PhD, UA associate professor of pharmacology and toxicology, was the corresponding author for the Science Advances paper, along with Dr. Chen as co-corresponding author. The work was supported in part by grants from the National Institutes of Health.
USF Health’s mission is to envision and implement the future of health. It is the partnership of the USF Health Morsani College of Medicine, the College of Nursing, the College of Public Health, the Taneja College of Pharmacy, the School of Physical Therapy and Rehabilitation Sciences, the Biomedical Sciences Graduate and Postdoctoral Programs, and USF Health’s multispecialty physicians group. The University of South Florida is a high-impact global research university dedicated to student success. Over the past 10 years, no other public university in the country has risen faster in U.S. News and World Report’s national university rankings than USF. For more information, visit health.usf.edu.
TDnews (tunisiesoir.com)