[ad_1]
There are more than 3 million cases of arthritis in the U.S. each year, and osteoarthritis is the most common type. In patients, cartilage — the slick surface on the ends of bones — wears away, bone rubs against bone, causing swelling and stiffness.
Now Keck School of Medicine of USC scientists in the USC Stem Cell laboratory of Denis Evseenko have collaborated with colleagues to offer new insights on how gene activity drives the development of cartilage. Their findings appear Friday in Nature Communications.
Based on their studies, the scientists identified and characterized, for the first time, unique cell populations that form the superficial zone of human joint cartilage. The zone has the most critical role in cushioning the joint and is often partially or completely lost in arthritis.
“Our results not only offer a unique molecular atlas of human skeletal development, but also define a strategy for joint cartilage repair,” said Evseenko, the study’s corresponding author and an associate professor of orthopedic surgery, and stem cell biology and regenerative medicine at the Keck School of Medicine.
Osteoarthritis research: gene activity of human cartilage cells
In a series of experiments, postdoctoral scholar-research associate Gabriel Ferguson and postdoctoral scholar-research associate Ben Van Handel and colleagues compared the gene activity of developing human cartilage cells with several other cell types.
First they compared the cartilage cells to four other types of developing human cells: the precursors to bone, muscle, tendon and ligament. As the cartilage matured, the genes specific to cartilage became increasingly active, while genes related to the other cell types became repressed.
The scientists then compared these developing human cartilage cells to equivalent cells from mice. The team found many broad similarities in gene activity.
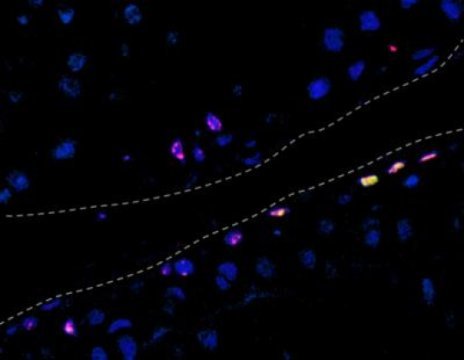
The researchers also carried out a detailed comparison of ordinary human cartilage cells and stem cell-derived human cartilage cells, taking into account genetics, genetic regulation and function. They demonstrated that stem cell-derived cartilage does not fully develop in the Petri dish but rather retains the genetic hallmarks typical of fetal cartilage. However, if the scientists transplanted stem cell-derived human cartilage at a particular stage of development into an arthritic rat, the cartilage would lose its fetal hallmarks and fully mature — regenerating the critical superficial zone.
Other authors were Maxwell Bay, Siyoung Lee, Ruzanna Shkhyan, Nicholas Banks, Mila Scheinberg, Biagio Saitta, Joseph Elphingstone and Michael Bonaguidi from USC; Petko Fiziev, April Pyle, Nicholas Bernthal, Hanna KA Mikkola and Jason Ernst from UCLA; Tonis Org from UCLA and the University of Tartu in Estonia; Ling Wu from InVitro Cell Research; and A. Noelle Larson, Scott Riester and Andre van Wijnen from the Mayo Clinic.
The study was supported by the National Institutes of Health (award number R01AR071734), the U.S. Department of Defense (award number W81XWH-13-1-0465) and the California Institute for Regenerative Medicine (award numbers RB5-07230-B and TRAN1-09288).
Story Source:
Materials provided by University of Southern California. Original written by Cristy Lytal. Note: Content may be edited for style and length.
[ad_2]