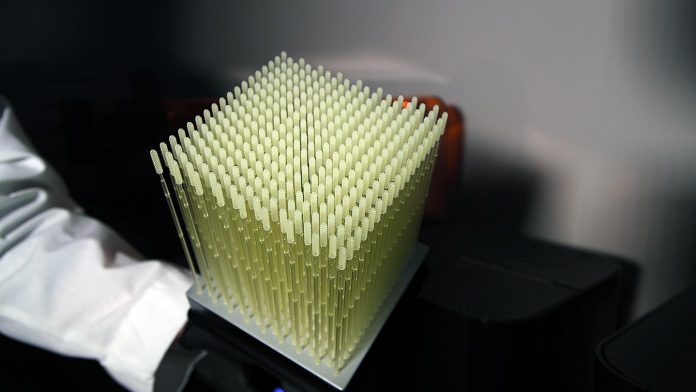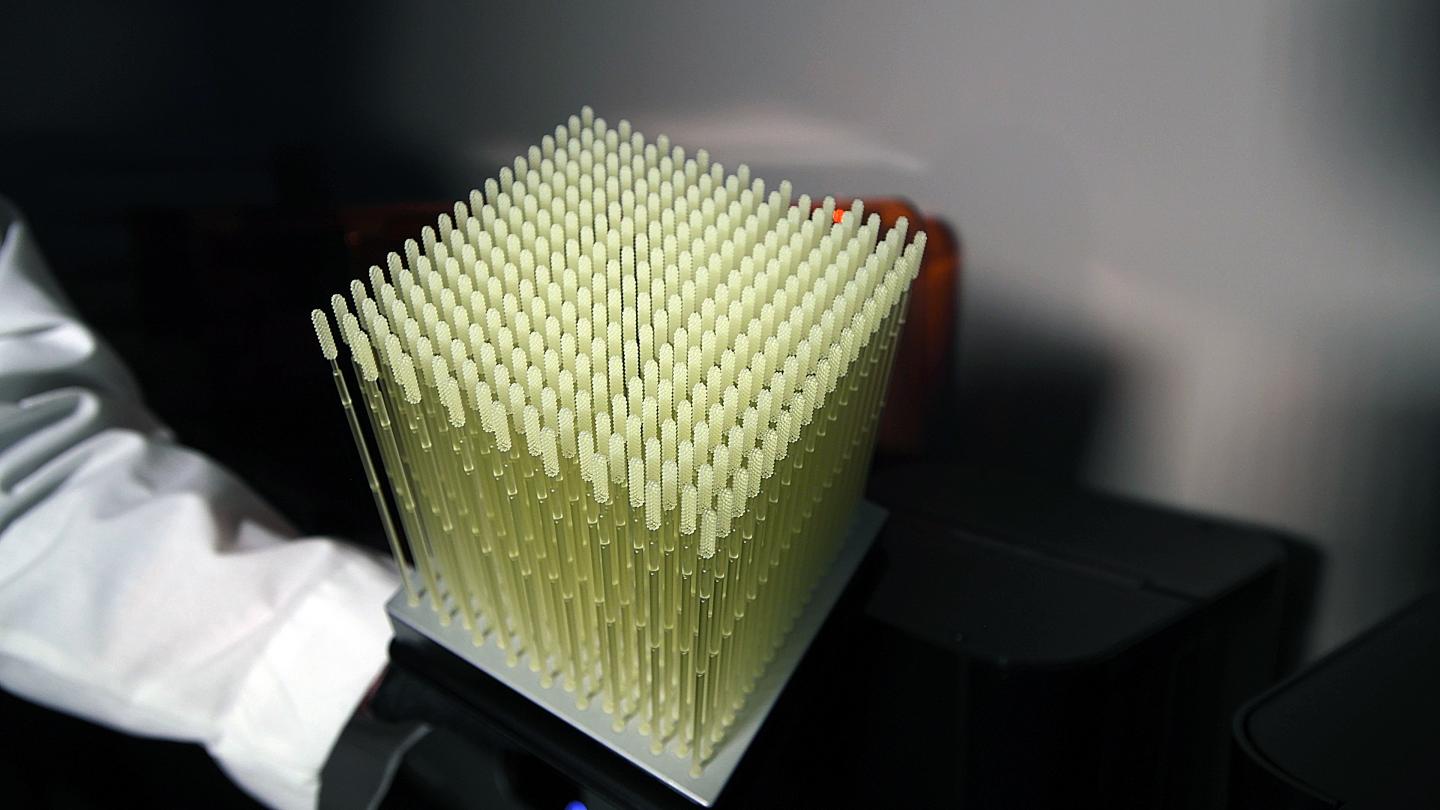
Photo: 3D printed swabs.
view more
Credit Image: Radiological Society of North America
OAK BROOK, Ill. – In response to the critical shortage of nasopharyngeal (NP) swabs early in the COVID-19 pandemic, the Department of Radiology at University of South Florida (USF) Health in Tampa set out to design, validate and create NP swabs using a point-of-care 3D printer. Results of the first clinical trial of 3D-printed NP swabs for COVID-19 testing are being presented at the annual meeting of the Radiological Society of North America (RSNA).
“To date, USF Health has printed more than 100,000 3D NP swabs, and hospitals around the world have used our 3D files to print tens of millions more swabs for point-of-care use,” said Summer Decker, Ph.D., associate professor, vice chair for research, and director of the 3D Clinical Applications for the Department of Radiology in the USF Health Morsani College of Medicine and Tampa General Hospital.
The 3D swab has received national and international recognition as an example of the power of medical 3D printing and quick innovation to provide clinical solutions.
The flocked NP swab, which collects a test sample of nasal secretions from the back of the nose and throat for lab analysis, is the current standard of care for diagnosing COVID-19. It consists of a narrow plastic rod and a tip covered in a flocked polyester material.
“COVID-19 appears first in the nasopharyngeal regions and from there it’s inhaled into the respiratory system,” Dr. Decker explained.
As the pandemic and demand for COVID-19 testing surged in early March, Dr. Decker and her team immediately began studying how they could develop an alternative to the flocked swab.
“We collaborated with our colleagues in infectious disease, virology, emergency medicine and radiology as well as Todd Goldstein, Ph.D., at Northwell Health System’s 3D Design and Innovation Lab in New York City. The city was the U.S. epicenter of virus infection at the time,” she said. “In a matter of days, we came up with 12 designs and printed three to test on ourselves.”
The final prototype, developed using FormLabs printers and surgical grade resin, was sent to infectious disease specialists at both USF and Northwell for validation testing.
“We needed to determine that the 3D NP swab could gather enough viral cells and hold them for up to three days, and that the resin would not interfere with test results,” she said.
To compare the performance of the 3D NP swab with the flocked swab, the USF Health team initiated a clinical trial at numerous sites including Tampa General Hospital, Northwell Hospital and Thomas Jefferson University Hospital in Philadelphia.
At the three trial sites, 291 patients (ages 14-94) who were hospitalized or seen in the emergency room were tested for COVID-19 using both the flocked swab and 3D swab. The 3D swab displayed statistically identical results to the flocked swab in the head-to-head trial.
“The results were overwhelmingly positive,” Dr. Decker said. “The clinical trial showed that the 3D nasal swabs performed as well as – or, in some cases, better than – flocked swabs.”
Tampa General Hospital adopted the 3D NP swab as its standard of care and began printing more than 300 swabs a day for the hospital and its affiliated care centers. The hospital’s six printers continue to print about 9,000 swabs per week.
The 3D printing process takes up to 15 hours depending on the printer. The printed swabs are rinsed in isopropyl alcohol, cured and hand-inspected for defects. Finally, a member of the hospital’s infectious disease team examines each swab before it is sterilized in an autoclave and packed in a test kit.
USF filed for a provisional patent on the 3D NP swab and provided the design files and clinical data at no cost to hospitals, clinics and licensed medical device companies around the world.
“We wanted to get this swab in as many hands as possible to help slow the spread of the virus,” Dr. Decker said. “This is the result of many people working together to make one device to help others.”
Dr. Decker notes that the project was initiated and developed through collaborations established in the RSNA 3D Printing Special Interest group.
“Medical 3D printing is housed in the field of radiology, and RSNA and the 3D Printing Special Interest Group give us a voice,” she said. “This project shows novel ways that radiology departments around the world can directly impact hospitals and clinical care during a crisis like COVID-19.”
###
Co-authors are Jonathan M. Ford, Ph.D., Sean Trahan, M.S., and Todd R. Hazelton, M.D.
For more information and images, visit RSNA.org/press20. Press account required to view embargoed materials.
RSNA is an association of radiologists, radiation oncologists, medical physicists and related scientists promoting excellence in patient care and health care delivery through education, research and technologic innovation. The Society is based in Oak Brook, Illinois. (RSNA.org)
Editor’s note:
The data in these releases may differ from those in the published abstract and those actually presented at the meeting, as researchers continue to update their data right up until the meeting. To ensure you are using the most up-to-date information, please call the RSNA media relations team at Newsroom at 1-630-590-7762.
For patient-friendly information on medical imaging and COVID-19, visit RadiologyInfo.org.
TDnews (tunisiesoir.com)