[ad_1]
Engineers at The University of Texas at Austin have developed a new noninvasive technique for simulating repairs to the heart’s mitral valve with levels of accuracy reliable enough for use in a clinical setting. Mitral valve (MV) disease is one of the most common valve-related heart conditions, newly diagnosed in 5 million Americans each year. Left unchecked, MV disease can lead to heart failure and/or stroke. This advance in computational modeling technology allows surgeons to provide patient-specific treatments, a development that will improve the long-term efficacy of current medical approaches.
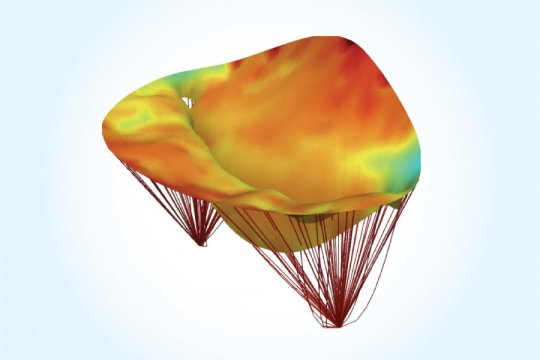
Led by Michael Sacks, a professor in the Department of Biomedical Engineering in the Cockrell School of Engineering, the team outlined their computational modeling technique for imaging MV leaflets — flaps located on the base of the valve that open and close to regulate blood flow from the left atrium to left ventricle of the heart — in recent issues of the International Journal for Numerical Methods in Biomedical Engineering and the Annals of Biomedical Engineering.
The MV plays a crucial role in maintaining healthy blood flow in the heart, but normal function can be compromised in a number of ways. For instance, heart attacks may disrupt the MV leaflets’ capacity to close properly, resulting in blood leaking back into the heart’s left atrium. The importance of healthy MV function is thus widely understood within the medical community, but there is not a consensus on how best to treat common MV disorders such as regurgitation, prolapse and mitral valve stenosis.
Until now, there has been a lack of accurate modeling approaches available to surgeons for predicting the best surgical methods to restore MV function.
“Heart valves are very difficult to study. They are complex structures that move incredibly fast and are located inside the heart, making them extremely difficult to image,” said Sacks, who also serves as director of the James T. Willerson Center for Cardiovascular Modeling and Simulation in the university’s Institute for Computational Engineering and Sciences. “Our new computational model provides surgeons with a tool for the prediction of postsurgical outcomes from clinically obtained presurgical data alone.”
Sacks has spent most of his academic career analyzing and modeling heart valve function. Recent advances in computational and 3D imaging technologies have made it possible for Sacks and his team to noninvasively and accurately acquire the in vivo (or living) geometry of the MV leaflets in patients from real-time 3D echocardiography — a clinical technique that uses sound waves to monitor heart function.
The UT team’s computational model was developed in collaboration with researchers from Penn Medicine and Georgia Tech.
“Our models combined the complete 3D geometry of the mitral valve in the open and closed states, making possible an unparalleled level of predictive accuracy,” Sacks said. “To model the MV leaflets, we then integrated into the MV models the structure and mechanical properties of the internal constituents, such as the collagen fibers which make up most of the valve, to develop attribute-rich complete MV models.”
Several studies have shown significant deficiencies in the long-term success of current surgical approaches to treating common heart valve diseases. Up to 60 percent of patients who have undergone MV regurgitation surgery report recurrence just two years after the surgery.
“Cardiac surgeons must decide upon the best possible treatment for heart valve repair without knowing all the facts,” said Dr. Robert Gorman, professor of surgery in the Perelman School of Medicine at the University of Pennsylvania and a key collaborator on the study. “Most rely on their own experiences or how they were taught to perform valve repair surgery in medical school.”
With the researchers’ new predictive technique, surgeons won’t have to take the previous one-size-fits-all approach to MV leaflet repair.
“The computational modeling tool we’ve developed will eliminate a lot of the uncertainty and allow for patient specificity,” Gorman said. “This will be transformative for those working in the field.”
The next step for Sacks and his research team is to commercialize their technique.
“Once heart surgeons gain access to this tool in a clinical setting, we anticipate significant improvements in the long-term well-being of patients who’ve undergone mitral valve surgery,” he said.
The study was funded by the National Institutes of Health.
Story Source:
Materials provided by University of Texas at Austin. Note: Content may be edited for style and length.
[ad_2]