[ad_1]
People living with cystic fibrosis (CF) spend their entire lives battling chronic lung infections that are notoriously resistant to antibiotic therapy. Yet a one-size-fits all approach to wiping out the offending bacterium may not be the best approach for all patients with the disease, according to a new study by researchers at University of California San Diego School of Medicine and Skaggs School of Pharmacy and Pharmaceutical Sciences.
Instead, researchers discovered that tweaking other factors in a CF lung model, such as pH balance and oxygen, helped eradicate pathogenic bacteria while minimizing risks of antibiotic resistance and overgrowth of other microorganisms.
The study is published September 26 in Science Advances.
“We think of antibiotics as causing a ‘scorched earth,’ simply wiping an unknown portion of both healthy and hopefully the bad bacteria. But we actually have a poor understanding of what happens to their microbiota when people take antibiotics — both healthy people and people with cystic fibrosis,” said Pieter Dorrestein, PhD, professor in the Skaggs School of Pharmacy and Pharmaceutical Sciences and departments of Pharmacology and Pediatrics in the School of Medicine and faculty leader in the Center for Microbiome Innovation at UC San Diego. Dorrestein led the study with Robert Quinn, PhD, who was an assistant project scientist at UC San Diego at the time of the study and is now an assistant professor at Michigan State University.
Due to the genetic defect that underpins CF, a thick, sticky mucus builds up in the lungs of patients with CF. The mucus helps microorganisms to thrive. One especially problematic bacterium, Pseudomonas aeruginosa, also forms a biofilm in the lung, which is difficult for the immune system and antibiotics to penetrate. These lung infections are a serious and chronic problem for many people living with CF. Currently, the infections are largely managed by trial-and-error with a combinations of antibiotics, antifungals and anti-inflammatory molecules.
“It’s amazing to think that disease management by expert clinicians (which we are not) largely via trial-and-error has increased the average lifespan for people with cystic fibrosis from two years in the 1930s to about 45 years in the U.S. and 55 years in Canada, and yet we have limited understanding of how such treatments affect the microbial communities living within people with cystic fibrosis,” Dorrestein said.
In biomedical research, scientists typically study bacterial infections by analyzing one specific type of bacteria, such as P. aeruginosa, and perhaps its interactions with human cells. But Quinn’s background is in environmental microbiology. He looks at the CF lung as a whole, living in a unique environment in which a particular bacterium doesn’t operate alone, but interacts with other microbes in the community, the human cells that make up the lung, as well as other molecules, chemicals and metabolites, and all of which behaves like an ecosystem.
So Quinn approached the lungs like he would any other environment, such as soil or ocean water. He developed a system he calls WinCF, named in part for 19th century microbial ecologist Sergei Winogradsky. Winogradsky invented a gradient system for studying microbes in soil. Likewise, Quinn’s WinCF system provides pH and oxygen gradients that mimic the narrow tubes that make up human lung bronchioles.
Quinn and team collected sputum samples from 18 patients with cystic fibrosis and applied them to the WinCF system in their lab. Then they altered factors such as pH, oxygen levels and antibiotics to map approximately 600 different cystic fibrosis lung conditions.
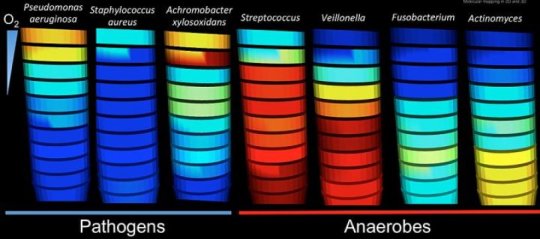
As a result of these pH and oxygen gradients, the researchers found that microbes in CF lungs divide themselves into two distinct communities: 1) known pathogens, microbes that can cause health problems, living in oxygen-rich regions and high pH and 2) anaerobes, microbes that thrive in areas low in oxygen and low pH.
“This stratification matters because it may affect treatments for cystic fibrosis patients,” Quinn said. “For example, certain bacteria may survive antibiotic treatment because they can hide deeper in the lung mucus. Meanwhile, the bacteria that are killed off may open up space for other microbes to grow, potentially creating a new set of problems.”
That’s what the researchers saw when they added the anti-P. aeruginosa antibiotic tobramycin to the top of the culture in their WinCF model, simulating inhalation into an airway with mucus-plugged bronchioles, as occurs in cystic fibrosis. The antibiotic caused drastic changes in the system’s microbial makeup. Some bacterial species were killed in all regions of the column, some killed in the higher, more oxygen-rich layers but survived at lower depths, while other species continued to thrive at the lower depth. Quinn said he was especially surprised to see blooms of Aspergillus fungi spring up in the regions previously occupied by the killed bacteria. Aspergillosis, the infection caused by this fungus, is not uncommon in cystic fibrosis patients treated with antibiotics.
Not only did the antibiotic shift the microbial balance in the cystic fibrosis lung model, the chemical structure of the antibiotic itself was modified by the microbes. This alteration could help bacteria resist its effect.
“Antibiotics alter the overall structure and relationships in a dynamic community, and not always in a way that’s beneficial for the patient,” Quinn said. “We don’t yet know the ‘rules’ for tipping the balance in favor of a beneficial microbial balance.”
In contrast, when the researchers simply lowered the pH of the cystic fibrosis mucus in the WinCF system by one unit, the bacterial makeup of the sample shifted from 70 percent P. aeruginosa to essentially none of those particularly troublesome bacteria.
“It may be that in some cases antibiotics may not even as effective as that simple pH change our laboratory experiment suggests, something worth exploring clinically,” Dorrestein said.
To be clear, the WinCF model is not a perfect replica of human cystic fibrosis lungs. It does not contain human cells or components of the immune system that would also help shape the real-life microbial makeup of a person’s lungs.
So while this system should not be used to influence patient care just yet, Dorrestein said the ultimate goal is a “precision-care” clinic for patients with cystic fibrosis. In this scenario, physicians and technicians could rapidly analyze each patient’s sputum for unique molecular and microbial patterns and test different combinations of treatment options in the lab — pH change, oxygen levels, antibiotics — before prescribing them to the patient.
[ad_2]