[ad_1]
One of the frontiers of medical diagnostics is the race for more sensitive blood tests. The ability to detect extremely rare proteins could make a life-saving difference for many conditions, such as the early detection of certain cancers or the diagnosis of traumatic brain injury, where the relevant biomarkers only appear in vanishingly small quantities.
Commercial approaches to ultrasensitive protein detection are starting to become available, but they are based on expensive optics and fluid handlers, which make them relatively bulky and expensive and constrain their use to laboratory settings.
Knowing that having this sort of diagnostic system available as a point-of-care device would be critical for many conditions, especially traumatic brain injury, engineers at the University of Pennsylvania have developed a test that uses off-the-shelf components and can detect single proteins with results in a matter of minutes, compared to the traditional workflow, which can take days.
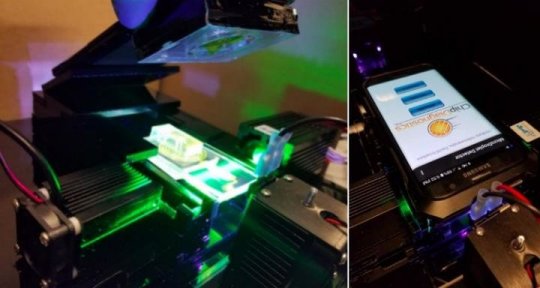
Using a standard cellphone camera and a set of strobing LED lights, combined with their lab’s microfluidic droplet generators, the team has developed a system that is a thousand times more sensitive than the standard protein assay, is handheld, and considerably less expensive than the current state-of-the-art single-protein tests first coming to market.
The researchers, led by David Issadore, assistant professor in Penn Engineering’s Department of Bioengineering, and graduate student Venkata R. Yelleswarapu, demonstrated their system in a study published in the Proceedings of the National Academy of Sciences.
The standard protein detection assay, ELISA, involves attaching antibodies to the proteins in question, then measuring how much the sample’s color changes in response to enzymes linked to the antibodies. This process is fast and simple enough to be incorporated in point-of-care devices, like home HIV tests, but only works when the proteins are in large concentrations.
There are currently very few biomarkers for traumatic brain injury because very few of the protein markers of those injuries make their way through the blood-brain barrier. Medical researchers have only recently confirmed that any such markers could be used for a blood test, and given their ultra-low concentrations, that test would need to be much more sensitive than the standard ELISA array.
“By a thousand times more sensitive,'” Issadore says, “we mean that if we had a vial of blood with only a few of the relevant proteins, we can accurately count those proteins, whereas a traditional test couldn’t reliably tell the difference between that vial of blood and one with none of the protein in it. As you keep increasing the number of proteins, the traditional test will eventually be able to detect them, but we can quantify the number of proteins at concentrations a thousand times less than they can.”
Issadore’s approach works by measuring one protein at a time, by breaking apart the sample into microdroplets, each of which contain either a single protein or none at all. His lab’s expertise in microfluidics has produced microchips etched with hundreds of microdroplet generators, all working in parallel.
“Normally, you’d have to measure very precisely how much a sample changes color or fluoresces, but here we’re turning it into tens of millions of yes-or-no questions,” Issadore says. “Digitizing that question brings down the cost of the camera and the surrounding fluid handling equipment, but shifts the problem into how to process tens of millions of those questions, in a way that is reproducible, accurate, inexpensive and portable.”
While an off-the-shelf camera can detect whether a microdroplet contains a fluorescent-marker-bound protein or not, the big challenge was to speed up the process. Existing digital droplet detectors line the droplets up so they can be measured one at a time. Such systems are accurate, but bulky and expensive. They also have limited throughput, because of the need to look at millions of droplets one at a time.
“A thousand droplets a second, the throughput of conventional technologies, is still pretty slow if you need to measure 50 million,” Yelleswarapu says.
Rather than having a single channel, the researchers flow droplets into hundreds of channels that pass by the camera at the same time. The bottleneck, however, is how fast a camera can capture the data.
“Conventionally, that wouldn’t work since the exposure time you’d get from a regular camera is such that the signals from two droplets next to each other would overlap,” Yelleswarapu says. “A cellphone camera takes about a hundred images a second, and that’s far too slow to be useful for us to resolve these droplets. But you can use that camera if the light source you’re using to illuminate the droplet strobes a thousand times faster than the framerate of the camera.”
The trick that makes the Issadore team’s approach work was to encode this strobing light with a signal that would allow them to tease apart one microdroplet from its neighbors.
“We’re strobing the light in a very specific pattern that never repeats itself, which is a technique we borrowed from radar,” Issadore says. “As the signals are going across the screen they get imprinted with this barcode. So even though they overlap with one another, we can tell them apart by which strobe pulse illuminated each droplet.”
Issadore’s group has previously published on traumatic brain injury markers, and has an ongoing research project with Presbyterian Hospital with brain injury patients. They also have a spin-off company, Chip Diagnostics, based at the Pennovation Center, which aims to produce test kits for early cancer diagnostics and traumatic brain injury.
[ad_2]