[ad_1]
Scientists from Waseda University, the National Defense Medical College, and the Japan Science and Technology Agency developed a new bioadhesive, wirelessly-powered light-emitting device which could better treat cancers in delicate organs.
Conventional photodynamic therapy induces cancer cell death by using photosensitizing agents, which localize in tumors and activate with exposure to a specific wavelength of light. In recent years, low-dose and long-term photodynamic therapy (metronomic photodynamic therapy, mPDT) has shown promise in treating cancers in internal organs. The problem with mPDT is, however, is that because the light intensity is extremely low (1/1000 of the conventional method), the antitumor effect cannot be obtained if the light source shifts even slightly away from the tumor, making the illumination insufficient.
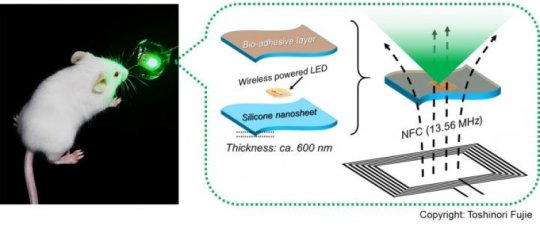
“To address this issue, we have developed a wirelessly-powered optoelectronic device that stably fixes itself onto the inner surface of an animal tissue like a sticker with bioadhesive and elastic nanosheets, enabling a continuous, local light delivery to the tumor,” says Toshinori Fujie, associate professor of biomedical engineering at Waseda University. The nanosheets are modified with the mussel adhesive protein-inspired polymer polydopamine, which can stabilize the device onto a wet animal tissue for more than 2 weeks without surgical suturing or medical glue. The light-emitting diode chips in the device are wirelessly powered by near-field-communication technology.
To test its effectiveness, tumor-bearing mice implanted with the device were injected with a photosensitizing agent (photofrin) and exposed to red and green light, approximately 1,000-fold intensity lower than the conventional PDT approaches, for 10 consecutive days. The experiment showed that the tumor growth was significantly reduced overall. Especially under green light, the tumor in some mice was completely eradicated.
Associate Professor Fujie points out, “This device may facilitate treatment for hard-to-detect microtumors and deeply located lesions that are hard to reach with standard phototherapy, without having to worry about the risk of damaging healthy tissues by overheating. Furthermore, because the device does not require surgical suturing, it is suitable for treating cancer near major nerves and blood vessels, as well as for organs that are fragile, that change their shape, or that actively move, such as the brain, liver, and pancreas.”
If clinically applied, the device could be beneficial for cancer patients who seek minimally invasive treatment, helping them live longer and improve their quality of life.
Story Source:
Materials provided by Waseda University. Note: Content may be edited for style and length.
[ad_2]