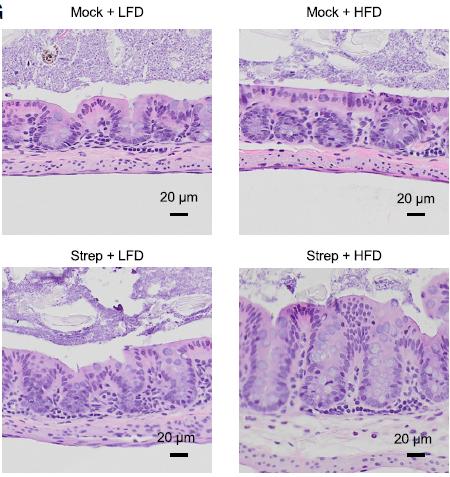
IMAGE: Image of sections of the colon’s inner lining, based on combinations of low-fat diet (LFD) vs. high-fat diet (HFD), and no treatment (mock) vs. with streptomycin (Strep) treatment….
view more
Credit: UC Davis Health
Irritable bowel syndrome (IBS) affects approximately 11% of people worldwide. It is characterized by recurring episodes of abdominal pain, bloating and changes in bowel habits. IBS patients with mucosal inflammation and changes in the gut’s microbial composition are considered pre-IBD.
Antibiotic usage with high-fat diet is a risk factor
The study included 43 healthy adults and 49 adult patients diagnosed with IBS. The researchers measured fecal calprotectin, a biomarker for intestinal inflammation, of participants. Elevated levels of fecal calprotectin indicated a pre-IBD condition. The study identified 19 patients with IBS as pre-IBD.
The researchers found that all participants who consumed high-fat diet and used antibiotics were at 8.6 times higher risk for having pre-IBD than those on low-fat diet and no recent history of antibiotic use. Participants with the highest fat consumption were about 2.8 times more likely to have pre-IBD than those with the lowest fat intake. A history of recent antibiotic usage alone was associated with 3.9 times higher likelihood of having pre-IBD.
“Our study found that a history of antibiotics in individuals consuming a high-fat diet was associated with the greatest risk for pre-IBD,” said Andreas Bäumler, professor of medical microbiology and immunology and lead author on the study. “Until now, we didn’t appreciate how different environmental risk factors can synergize to drive the disease.”
Shutting the cell’s powerhouse promotes gut microbial growth
Using mouse models, the study also tested the effect of high-fat diet and antibiotics use on the cells in the intestinal lining. It found that high-fat diet and antibiotics cooperate to disrupt the work of the cell’s mitochondria, shutting its ability to burn oxygen. This disruption causes reduction in cell’s oxygen consumption and leads to oxygen leakage into the gut.
The body’s beneficial bacteria thrive in environments lacking oxygen such as the large intestine. Higher oxygen levels in the gut promote bacterial imbalances and inflammation. With the disruption in the gut environment, a vicious cycle of replacing the good bacteria with potentially harmful proinflammatory microbes that are more oxygen tolerant begins. This in turn leads to mucosal inflammation linked to pre-IBD conditions.
The study also identified 5-aminosalicylate (mesalazine), a drug that restarts the energy factories in the intestinal lining, as a potential treatment for pre-IBD.
“The best approach to a healthy gut is to get rid of the preferred sustenance of harmful microbes,” Lee said. “Our study emphasized the importance of avoiding high fat food and abuse of antibiotics to avoid gut inflammation.”
###
Co-authors on this study are Stephanie Cevallos, Mariana Byndloss, Connor Tiffany, Erin Olsan, Brian Butler, Briana Young, Andrew Rogers, Henry Nguyen, Kyongchol Kim, Sang-Woon Choi, Eunsoo Bae, Je Hee Lee, Ui-Gi Min and Duk-Chul Lee.
This work was supported by the National Research Foundation of Korea grant
(NRF-2017R1C1B5016190), USDA/NIFA award 2015-67015-22930 and by the Public Health Service grants AI044170, AI096528, AI112445, AI112949, AI060555 and 5TL1R001861.
Lee et al., High-Fat Diet and Antibiotics Cooperatively Impair Mitochondrial Bioenergetics to Trigger Dysbiosis that Exacerbates Pre-inflammatory Bowel Disease, Cell Host & Microbe (2020), https:/
s.edu/health-news/newsroom/ibd-what-it-is-and-how-to-control-it/2019/04














