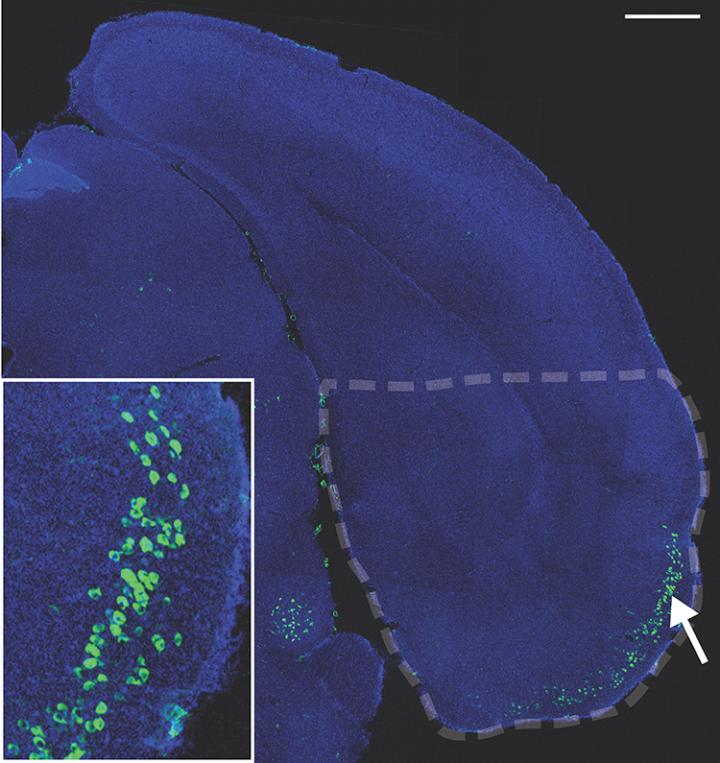
IMAGE: Principal neurons of the entorhinal cortex layer II assist with memory and navigation and are among the most vulnerable to Alzheimer’s. Researchers generated a line of mice for studying ECII…
view more
Credit: J.-P. Roussarie et al./Neuron 2020
Neurons that regularly remodel are more prone to Alzheimer’s disease and die when that remodeling goes awry, a new study suggests. The work is the first to track the progression of Alzheimer’s at the genetic and molecular levels within neurons vulnerable to the disease.
“Identifying the molecular characteristics of neurons that are especially vulnerable to neurodegeneration is important both for the basic understanding of Alzheimer’s and for future development of better diagnostic and treatment options,” says study co-author Olga Troyanskaya, deputy director for genomics at the Flatiron Institute’s Center for Computational Biology in New York City and a professor at Princeton University.
Using a machine learning framework that integrated neuron type-specific mouse experiments with human studies, the researchers compared two types of neurons susceptible to Alzheimer’s with five resistant types. The most significant difference was that the vulnerable neurons were enriched with processes related to remodeling connections with adjacent neurons.
The findings suggest that aging and the accumulation of a protein fragment called amyloid-beta can cause the remodeling process to go haywire, creating tangles of tau proteins that lead to neuron death. The work is the first to link amyloid-beta and tau proteins — two previously proposed prime suspects in Alzheimer’s progression — at the genetic and molecular levels.
“By understanding what makes these neurons extra vulnerable, we can understand what makes Alzheimer’s start killing neurons,” says study co-lead author Vicky Yao, an assistant professor of computer science at Rice University in Houston who started the project while working in Troyanskaya’s group at Princeton. “The question now is whether we can somehow make these neurons more resistant.”
Yao led the work along with Jean-Pierre Roussarie, a senior research associate at the Fisher Center for Alzheimer’s Disease Research at Rockefeller University in New York City. The researchers present their findings June 29 in Neuron.
Alzheimer’s is a progressive disorder that causes brain cells to waste away and die. The disease first targets neurons related to memory and navigation. Over time, the disease spreads to other neurons. In the United States, Alzheimer’s is the sixth-leading cause of death and the fifth-leading cause of death for Americans age 65 and older.
The cause of the disease remains unclear. Previous studies identified genes that elevate Alzheimer’s risk, but scientists still don’t know why the disease starts attacking neurons. One challenge to studying the disease is that the brain quickly starts deteriorating after death, distorting any potential postmortem findings.
For the new study, Roussarie and his colleagues generated genetic lines of mice tailor-made for studying neurons. Each line focuses on a single neuron type, with genetic changes to make gene transcription in those neurons easier to track (including the addition of a green fluorescent protein). The researchers developed mice lines targeting neurons resilient to Alzheimer’s and others targeting neurons vulnerable to the disease.
In the new paper, the researchers show that the human and mouse neurons were nearly identical at the molecular level, making the rodents superb stand-ins for studying Alzheimer’s.
The researchers combined experimental data from Roussarie’s mice with Yao’s computational models of human genetics, which show when and where genes related to Alzheimer’s-related processes are expressed in the brain and how those genes interact with other genes. Together, the two data sources produced a profile of what characteristics make neurons vulnerable to Alzheimer’s.
The profile turned up two of the usual suspects in Alzheimer’s: amyloid-beta and tau. Amyloid-beta is a protein fragment that can aggregate, forming plaques that fill the gaps between nerve cells. Tau proteins — the top candidate in the profile — stabilize microtubules, molecular rods that give neurons their shape and form the backbone of connections between neighboring neurons. When tau proteins are misfolded, they can create tangled threads that block a neuron’s transport system, preventing neurons from functioning properly.
“When I first did the predictions, I actually went back and double-checked because I thought that this was too good to be true,” Yao says. “These were things we had already known were related to Alzheimer’s, and we were able to link them together. It was verification that we were on the right track.”
Scientists have long debated which process — involving amyloid-beta or tau — is responsible for the onset of Alzheimer’s, but the new findings suggest that the two are connected. The work strongly linked PTB, a gene that regulates the formation of the several flavors of the tau protein, to Alzheimer’s. If PTB is dysregulated, the ratio of tau proteins is thrown off. This imbalance causes the tau proteins to start aggregating, forming the tangled threads. The researchers propose that age and amyloid-beta accumulation boost the risk of this dysregulation.
The researchers plan to continue their research by looking for other characteristics that make neurons vulnerable to the disease. Gathering more information about the onset of Alzheimer’s will aid the development of potential treatments that prevent the disease from taking root in the first place, Yao says.
TDnews














