UCLA researchers have discovered how adult stem cells contribute to the development of lung cancer. The results of the three-year study may lead to personalized treatments to prevent lung cancer from developing in individuals at risk.
A research team led by Dr. Brigitte Gomperts, a member of UCLA’s Jonsson Comprehensive Cancer Center and the Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research, has discovered how processes that regulate growth of adult stem cells can lead to the development of precancerous lesions. These stem cells are involved in the regeneration of lung tissue that has been damaged. This process is considered to be the first stage in the development of lung cancer.
The investigators note that their findings have the potential to develop new personalized treatments for lung cancer, which causes an estimated 29% of all cancer deaths per year in the US. The authors note that adult stem cells are present in lung airways to specifically repair them after injury or disease (e.g., from smoking, air pollution, or a virus infection). They found that this reparative process is highly regulated by molecules known as reactive oxygen species, or ROS.
Recent studies have reported that low levels of ROS signal the stem cells to perform important cellular functions such as dividing and repairing; in contrast, high levels of ROS can be toxic to stem cells and destroy them. Controversy exists regarding what level of ROS is required for the repair process to be initiated. The investigators found that it is the dynamic flux of ROS from low to moderate levels in the airway stem cells that stimulates the repair process. In addition, the study revealed that the increase in ROS levels during cell repair is promptly reduced to low levels to prevent excessive cell proliferation (growth).
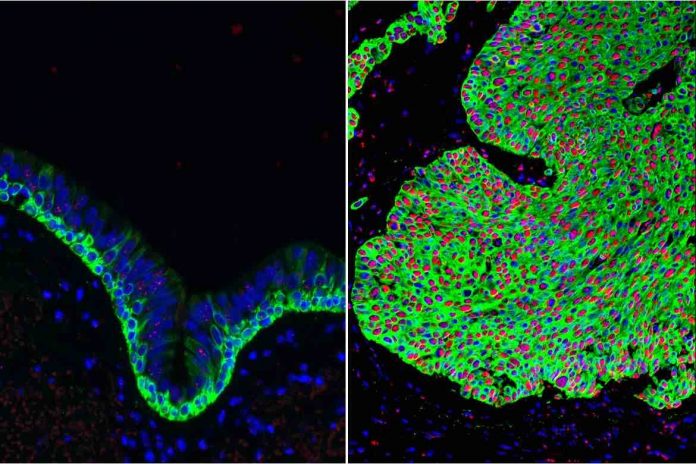
The researchers discovered that the disruption of this normal regulation of ROS back to low levels is comparable to removing the brakes from the stem cells. Under these circumstances, the stem cells will continue to make too many copies of themselves and not mature; thus, they become cancerous growths. Cancer is thought to develop in a stepwise fashion; thus, progressive genetic changes to the cells in these lesions over time can result in the development of malignant tumors.
“Low ROS is what keeps stem cells in a ready state so that your body is poised and ready to respond to injury and repair,” explained Dr. Gomperts. She added, “Loss of this ROS regulation leads to precancerous lesions. Now, with this pre-cancerous model in place, we can begin looking for what we call driver mutations, or those specific changes that take the pre-cancerous lesions to full-blown cancer.” She noted that many exposures exist that that can cause an increase in ROS in airway stem cells; thus, promoting cancer development. These include cigarette smoke, smog, and bacteria.
Dr. Gomperts noted, “There are likely multiple ways for a patient to get to a precancerous lesion, so the process could be different amongst different groups of people. Imagine a personalized way to identify what pathways have gone wrong in a patient, so that we could target a therapy to that individual.” The authors noted that the development of techniques to determine effective drug molecules, such as high-throughput screening systems to screen large libraries of compounds has great potential for future research to prevent precancerous growths from developing; thus, leading to innovative new cancer prevention strategies. The study also consolidates similar research by others because it finally identifies specifically how ROS affects the propagation of stem cells.