In the United States, coronary heart disease (CHD); the most common type of heart disease is the leading cause of death of men and women. One in four women dies from heart disease and around 64% of women who die suddenly from CHD had no previous symptoms.
CAD’s impact on women traditionally has been underappreciated due to higher rates at younger ages in men. Microvascular coronary disease greatly affects women. Women have unique risk factors for CAD, including those related to pregnancy and autoimmune disease, according to a new review by Dr. Martha Gulati, MD, MS, FACC, FAHA, associate professor of medicine and Dr. Kavita Sharma , MD, assistant professor clinical, cardiovascular medicine, both from Ohio State University, Columbus.
In addition they note that women are less likely to receive preventive recommendations such as lipid-lowering therapy, aspirin and lifestyle advice,
In their review the authors summarized “The manifestation of CAD has unique characteristics in women. Increasing data demonstrate that some treatment strategies have sex-specific effectiveness.”
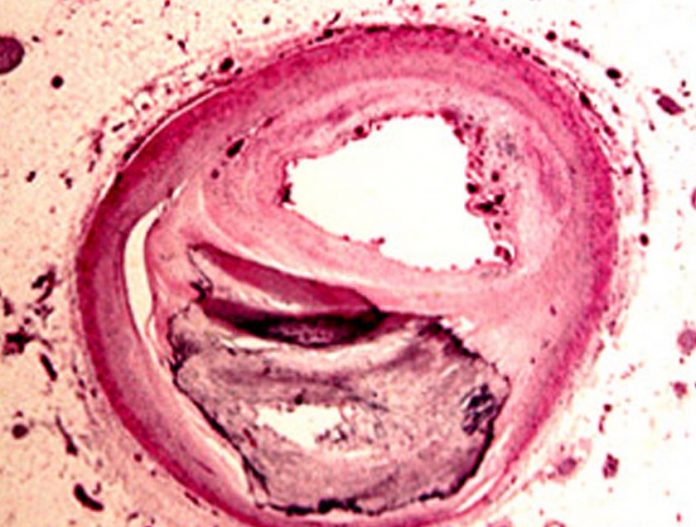
CT scans and other imaging techniques show that women have narrower coronary arteries than do men, and are more likely to suffer CAD due to microvascular disease. So while appearing not to have major coronary artery obstructions, women suffer symptoms due to blockages of these smaller vessels. Over one-half of symptomatic women without obstructive CAD continue to have signs and symptoms of ischemia and to undergo repeat hospitalization and coronary angiography.
They also reported women have greater incidence of coronary plaque erosion, while men are more likely to have obstructed CAD (narrowing or blockage in the coronary arteries) is more commonly found in men who are symptomatic and can be treated with aggressive medical therapy or stenting. This type of CAD is less frequently seen in women.
Pooled estimates from multiple countries revealed that women, both pre- and postmenopausal, are also 20% more likely to suffer angina than men.
Women are more likely to have autoimmune diseases then men in which raises their risk of CAD.
Exclusive to women are hormonal changes that occur over their lifetime and eventually affect CAD risk. Dysfunction in ovulation has been associated with increased CAD risk. A history of pre-eclampsia or gestational diabetes categorizes a woman as “at risk” for CAD, based on “Effectiveness-Based Guidelines for Prevention of CAD in Women.” Another risk factor to consider in women is the effect of breast cancer therapy on future CAD risk. As was recently reported, although advances in breast cancer therapies are improving survival in early breast cancer, the gains are being attenuated by increasing CAD risk. Diabetes increases a woman’s risk of CAD by 3-7 times, while for men it is only 2-3 times. And a diabetic woman is 3 times more likely to develop CAD than a non-diabetic woman.
Traditional risk factors such as age, family history of CAD, hypertension, diabetes, dyslipidemia, smoking, and physical inactivity are important predictors of risk in women. In contrast to the linear increase in CAD in men as they age, there is a more exponential increase in CAD in women after the age of 60.
Another critical risk factor is lack of physical fitness. Women unable to carry out basic fitness tests were three times more likely to develop CAD than fitter women. Increasing physical activity is a key component of the World Heart Federation’s ‘Make a Healthy Heart Your Goal’ campaign, running in partnership with this month’s Women’s European Football Championships. Heart disease in women will also be a major focus of WHF’s World Heart Day, which takes place on September 29. Furthermore, part of WHF’s overall strategy is aligned with that of WHO to reduce premature mortality related to non-communicable diseases, including CVD, by 25% by 2025, noted the researchers.
Among patients undergoing coronary artery bypass grafting (CABG), however, female sex is an independent risk factor for morbidity and mortality. Women have a higher risk of morbidity and mortality and they experience less relief from angina than do men after CABG, despite comprising less than 30% of the CABG population.
In their summary the researchers write “Women are affected by CAD in large numbers and to a large degree. CAD is the leading cause of mortality in women. The manifestation of CAD has unique characteristics in women. Increasing data demonstrate that some treatment strategies have sex-specific effectiveness. Further research regarding the pathophysiology of CAD in women, diagnosis, and treatment strategies specific to women is required. CAD is not a “man’s only” disease, and we eagerly await future studies that examine its unique presence in women”.