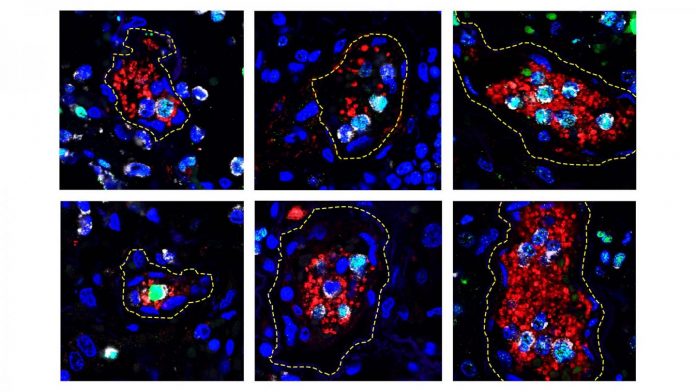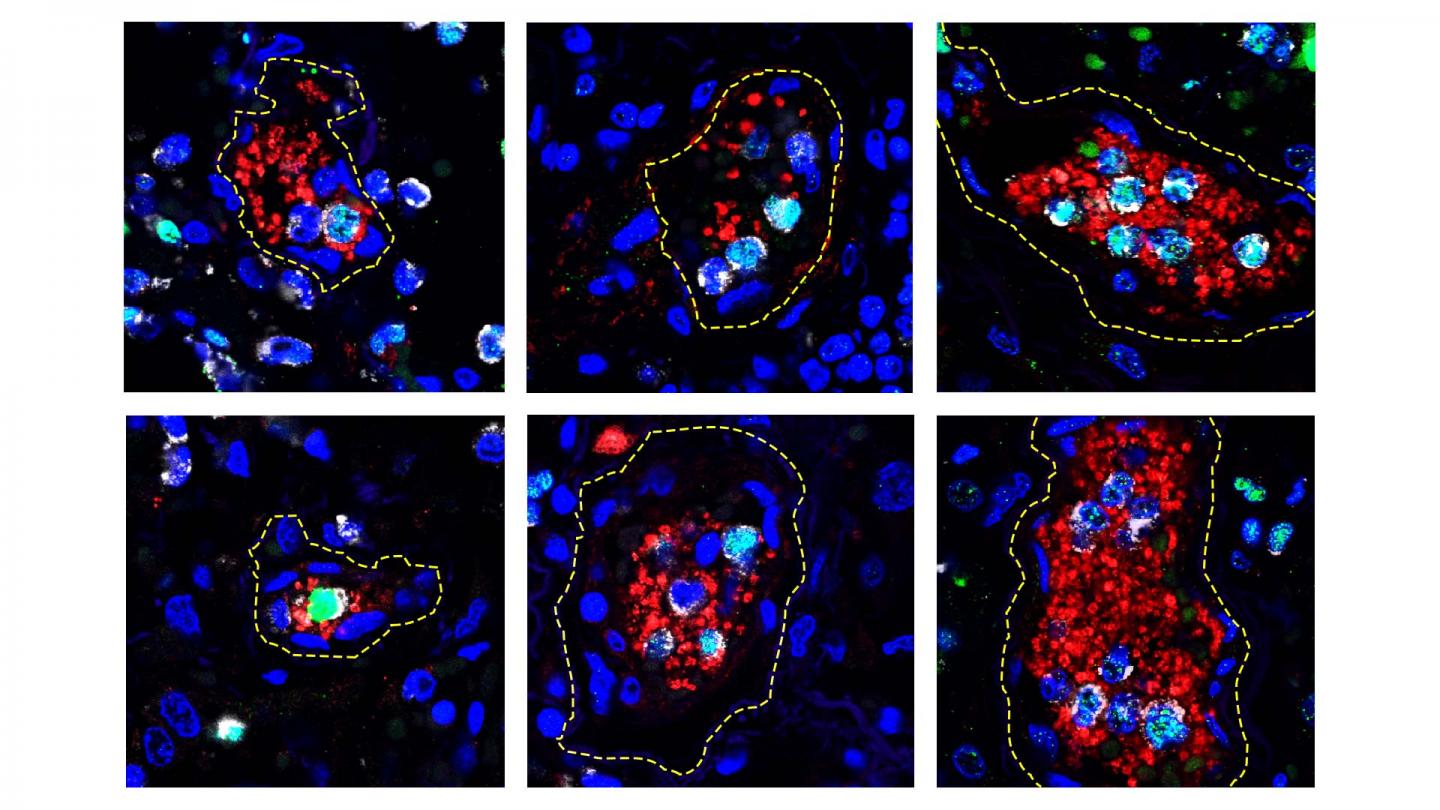
IMAGE: Photomicrographs of human lung tissue taken from a patient who died of COVID-19. These are examples of the Neutrophil Extracellular Trap (NET) structures associated with small blood clots. Small blood…
view more
Credit: Xue-Yan He and David Ng, Egeblad Lab/CSHL, 2020
Scientists have new evidence that overactive neutrophils–a common type of circulating immune cell–may drive the life-threatening blood clots and inflammation that occur in some patients with COVID-19. High levels of the sticky, pathogen-trapping webs produced by the cells were associated with the most severe cases of COVID-19 in a study reported online in the journal Blood.
Neutrophil extracellular traps (NETs) are a type of defense that the immune system deploys against certain pathogens–webs of DNA and toxins that ensnare and destroy viruses and bacteria. When too many of these NETs accumulate during a persistent infection, they can lead to acute respiratory distress syndrome, which leads many patients with COVID-19 to require intensive care.
Researchers at Cold Spring Harbor Laboratory (CSHL), University of Utah Health, PEEL Therapeutics and Weill Cornell Medicine collaborated to investigate NETs suspected role in COVID-19, collecting blood samples from 33 hospitalized patients, as well as autopsy tissue. They found that biomarkers of NET formation were more abundant in patients who required ventilation, and highest in the three study participants who eventually died from COVID-19.
When the team examined the lungs of the patients who died, they found tiny clots of tangled NETs and blood platelets known as microthrombi scattered through the tissue. “It will be important to investigate NETs role in clot formation (thrombosis) not only in light of the COVID-19 pandemic, but also to understand their broader role in disease,” says CSHL Associate Professor Mikala Egeblad.
“Excess NETs are formed in other viral diseases,” she says. “We also know that clotting is a major cause of death in people with end-stage cancer, so what we are learning in COVID-19 may help us understand basic properties in cancer and other diseases.”
In the laboratory, neutrophils from patients with COVID-19 churned out exceptionally high levels of NETs, and the researchers found healthy neutrophils behaved the same way when they were exposed to plasma from patients with the illness. They could stop NET production, however, by exposing cells to neonatal NET-Inhibitory Factor (nNIF), an anti-inflammatory peptide from umbilical cord blood that protects newborn babies.
Several therapeutic strategies for dismantling NETs or preventing their formation are currently under investigation. These include the nNIF peptide, which is in pre-clinical development by PEEL Therapeutics. “Although further studies will be required, the NET-inhibitory protein may block exaggerated NET formation in COVID-19 patients,” says Christian Con Yost, whose laboratory at University of Utah Health discovered nNIF in 2016.
###
TDnews